How I Finally Tamed My Insomnia — A Real Long-Term Health Journey
For years, sleep felt like a distant memory—tossing, turning, and watching the clock tick past 3 a.m. I tried quick fixes, but nothing lasted. What changed? A shift in how I saw sleep, not as a problem to fix, but as part of my overall health management. This isn’t about overnight miracles—it’s about small, consistent changes that add up. If you’re tired of being tired, this long-term approach might be what finally works.
The Hidden Cost of Chronic Sleeplessness
Insomnia is often reduced to a simple inability to fall asleep, but its effects ripple far beyond restless nights. It is not just about feeling groggy in the morning; it is a systemic disruption that impacts energy, mood, cognitive function, and long-term physical health. When sleep becomes inconsistent or insufficient, the body struggles to repair tissues, regulate hormones, and support immune function. Over time, chronic sleeplessness increases the risk of conditions such as hypertension, type 2 diabetes, and cardiovascular disease. The brain, deprived of its nightly reset, becomes less efficient at processing emotions and managing stress, which can lead to heightened anxiety and irritability.
One of the most overlooked consequences of poor sleep is its effect on the immune system. Research shows that people who consistently get less than six hours of sleep per night are more susceptible to infections like the common cold. This happens because sleep supports the production of cytokines—proteins that help the immune system fight off inflammation and infection. Without adequate rest, this defense mechanism weakens. Additionally, sleep disruption interferes with the balance of key hormones such as cortisol, insulin, and leptin. Cortisol, the stress hormone, can remain elevated, making relaxation more difficult. Insulin sensitivity decreases, raising blood sugar levels, while leptin, which regulates appetite, becomes dysregulated—often leading to increased hunger and weight gain.
Perhaps the most critical shift in understanding insomnia is recognizing it not as a standalone issue but as a symptom of deeper imbalances. For many, sleep problems are tied to lifestyle patterns, mental health, or undiagnosed medical conditions. Treating insomnia only with sleep aids or behavioral tricks, without addressing root causes, is like putting a bandage on a wound that continues to bleed. Long-term improvement requires a holistic view—one that considers daily routines, emotional well-being, and physical health as interconnected pieces of the sleep puzzle. When approached this way, better sleep becomes not just a goal, but a natural outcome of a more balanced life.
Why Quick Fixes Fail: The Myth of the Magic Solution
In the search for relief, many turn to quick fixes—over-the-counter sleep aids, a glass of wine before bed, or the glow of a smartphone screen to distract the mind. These strategies may offer temporary comfort, but they rarely lead to lasting change. In fact, they often make the problem worse over time. Sleep medications, even those available without a prescription, can create dependency. The body may begin to rely on these substances to initiate sleep, making it harder to fall asleep naturally when they are not used. Moreover, many of these drugs alter sleep architecture, reducing the amount of deep, restorative sleep and increasing light sleep stages, which leaves a person feeling unrested despite spending hours in bed.
Alcohol is another common but misleading sleep aid. While it may help someone fall asleep faster, it disrupts the second half of the sleep cycle. As alcohol is metabolized, it causes frequent awakenings, suppresses REM sleep, and can trigger snoring or breathing irregularities, especially in people prone to sleep apnea. The result is fragmented, low-quality sleep that fails to restore energy or support cognitive function. Similarly, using screens to unwind—scrolling through social media or watching videos—may seem harmless, but the blue light emitted by devices suppresses melatonin, the hormone that signals it’s time to sleep. This delays the body’s natural wind-down process and pushes the circadian rhythm later, making it harder to fall asleep at a reasonable hour.
The appeal of quick fixes lies in their immediacy, but they ignore the underlying habits and conditions that contribute to insomnia. They treat the symptom without changing the system. A more effective approach requires patience and consistency—building daily routines that support natural sleep onset and maintenance. This means replacing short-term crutches with sustainable practices: consistent wake-up times, exposure to morning light, mindful eating, and stress-reduction techniques. These changes may not produce dramatic results overnight, but they create the conditions for sleep to return as a natural, reliable rhythm rather than a battle to be won each night.
Rewiring My Routine: Building a Sleep-Ready Lifestyle
One of the most transformative realizations in my journey was understanding that sleep doesn’t start at bedtime—it begins the moment I wake up. The body operates on a circadian rhythm, a 24-hour internal clock regulated by light, activity, and routine. When this rhythm is aligned with natural environmental cues, sleep becomes easier and more restful. But modern life—irregular schedules, artificial lighting, and constant stimulation—often throws this system out of balance. To restore healthy sleep, I had to rebuild my daily routine with intention, focusing on consistency and timing.
The first change I made was committing to a consistent wake-up time, even on weekends. This might seem small, but it anchors the circadian rhythm. When the body expects to wake up at the same time every day, it begins to release cortisol naturally in the morning, which promotes alertness, and melatonin in the evening, which prepares the body for sleep. I also made it a priority to get exposure to natural light within 30 minutes of waking. Whether it was a short walk outside or sitting by a sunny window, this simple act helped signal to my brain that the day had begun, reinforcing the natural light-dark cycle.
Meal timing became another key factor. I noticed that eating late at night, especially heavy or spicy foods, made it harder to fall asleep. Digestion slows during sleep, and a full stomach can lead to discomfort or acid reflux. By shifting dinner to earlier in the evening and avoiding large snacks after 8 p.m., I reduced nighttime disturbances. I also paid attention to caffeine intake, limiting it to the morning hours and avoiding it after noon. While tea or coffee might feel harmless in the afternoon, caffeine has a half-life of up to six hours, meaning it can still be active in the system at bedtime, even if its stimulating effects aren’t immediately felt.
Physical activity played a supporting role as well. Regular exercise, particularly in the morning or afternoon, helped reduce stress and improve sleep quality. However, I learned that intense workouts too close to bedtime could be counterproductive, as they raised body temperature and adrenaline levels. Instead, I shifted vigorous activity to earlier in the day and reserved evenings for gentler movement like stretching or walking. These adjustments didn’t fix my insomnia overnight, but they created a foundation—small, daily habits that gradually shifted my body back into a natural rhythm.
Creating a Nightly Ritual That Actually Works
If daytime habits set the stage for sleep, the evening routine determines whether the curtain rises smoothly. I used to underestimate the power of a consistent wind-down process, thinking that as long as I was tired, sleep would follow. But the brain needs time to transition from the busyness of the day to the stillness of sleep. Without a deliberate routine, it remained in 'active mode' long after I climbed into bed. To change this, I built a nightly ritual focused on calming the nervous system and signaling safety to the body.
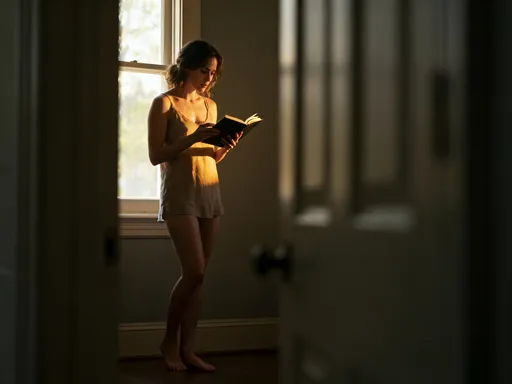
The first step was a digital detox. I set a 45-minute screen curfew before bed, turning off phones, tablets, and the television. This not only reduced blue light exposure but also minimized mental stimulation from emails, news, or social media. Instead, I replaced screen time with low-light, low-stimulation activities: reading a physical book, listening to soft music, or doing a simple skincare routine. These actions became cues—like Pavlov’s bell—that told my brain it was time to slow down.
Temperature also played a surprising role. I learned that the body’s core temperature naturally drops in the evening to prepare for sleep. A warm shower or bath about an hour before bed helped accelerate this process. As the body cooled down after the warmth, it mimicked the natural temperature dip, making me feel drowsy. I also adjusted the thermostat in my bedroom, keeping it slightly cool—around 65–68 degrees Fahrenheit—which research shows is optimal for sleep onset and maintenance.
My sleep environment received a thorough review. I invested in blackout curtains to block outside light, used a white noise machine to mask sudden sounds, and ensured my mattress and pillows provided proper support. Even small details mattered: I kept the room clutter-free and used calming scents like lavender in a diffuser, which some studies suggest may help reduce anxiety and improve sleep quality. These changes transformed my bedroom from a multipurpose space into a sanctuary dedicated solely to rest. Over time, just entering the room began to trigger a sense of calm, reinforcing the mental association between the space and sleep.
Mind Over Midnight: Managing the Mental Blocks to Sleep
Even with the perfect environment and routine, the mind can be the greatest barrier to sleep. For years, my biggest struggle wasn’t physical restlessness—it was mental hyperactivity. Lying in bed, my thoughts would race: replaying conversations, worrying about tomorrow, or analyzing why I couldn’t sleep. This mental loop only heightened anxiety, making sleep feel like a performance I was failing. I realized that calming the mind was not about stopping thoughts—impossible for anyone—but about changing my relationship with them.
I began using cognitive techniques to manage nighttime overthinking. One of the most helpful was thought labeling. When a worry arose—“What if I don’t get enough sleep for work tomorrow?”—I would silently name it: “That’s a worry about productivity.” This simple act created distance, turning the thought from a command into an observation. Another tool was worry journaling. About 30 minutes before bed, I would write down any lingering concerns, along with a brief note on how I might address them the next day. This practice helped me “park” the thoughts outside my head, reducing the urge to rehearse them in bed.
Perhaps the most powerful shift was learning acceptance. I stopped treating sleep as something I had to force or achieve. Instead, I focused on creating the conditions for rest and letting go of the outcome. I reminded myself that even if I didn’t fall asleep right away, lying quietly with my eyes closed still offered some restoration. This reduced the pressure and, paradoxically, made sleep more likely to come. Over time, I came to see mental calm not as an instant switch but as a skill—like learning to play an instrument or speak a new language—that improves with practice, patience, and consistency.
Tracking Progress Without Obsession: Tools for Long-Term Awareness
In any health journey, awareness is key—but so is balance. I wanted to understand my sleep patterns without becoming obsessed with data. Early on, I tried tracking every night in a notebook, recording when I went to bed, when I fell asleep, how many times I woke up, and how I felt in the morning. This helped me spot trends: I noticed that nights after stressful days or late meals were more disrupted, while consistent wake-up times led to better overall rest. However, I soon realized that over-monitoring could backfire. Fixating on the numbers made me anxious, turning sleep into a test I had to pass.
I adjusted my approach, shifting from rigid tracking to gentle reflection. Instead of logging every detail, I began asking myself a few simple questions each morning: How rested do I feel on a scale of 1 to 10? Was my mood stable? Did I have steady energy? These subjective measures were often more telling than exact sleep durations. I also paid attention to non-sleep indicators: was I more patient with my family? Did I make better food choices? These signs suggested that even small improvements in rest were having ripple effects on my overall well-being.
I experimented with wearable sleep trackers but used them sparingly. While they provided interesting insights—like trends in heart rate variability or sleep stages—I didn’t let the data dictate my self-worth. I learned that these devices are estimates, not medical-grade measurements, and can sometimes misinterpret restful wakefulness as poor sleep. The goal wasn’t perfection but pattern recognition: identifying what generally supported better rest and what didn’t. This mindset helped me stay curious rather than critical, focused on progress rather than performance.
Sleep as Self-Care: Making It Part of Lifelong Health Management
The final and most profound shift was reframing sleep not as a luxury or an afterthought, but as a cornerstone of health. In a culture that often glorifies busyness and productivity, rest can feel like indulgence. But the truth is, sleep is not downtime—it is active maintenance. It is when the brain consolidates memories, the body repairs cells, and the immune system regenerates. Prioritizing sleep is not selfish; it is an act of self-respect and long-term investment.
As my sleep improved, I noticed changes that extended far beyond the bedroom. My decision-making became clearer, my emotions more balanced, and my energy more stable throughout the day. I found myself making healthier food choices, exercising more consistently, and engaging more patiently with loved ones. These benefits reinforced the importance of treating sleep as foundational, not optional. It became less about fixing insomnia and more about nurturing a lifestyle that naturally supports rest.
This journey taught me that sustainable change doesn’t come from a single breakthrough but from daily commitment. There are still nights when sleep is elusive, but I no longer panic. I return to my routines, adjust what I can, and trust the process. Sleep is not a problem to be solved but a rhythm to be honored. By integrating it into my overall health management—with kindness, consistency, and awareness—I’ve built a resilience that lasts. And in that quiet, hard-won peace, I’ve finally found rest.